Infant feeding and child health
“There is no finer investment for any community than putting milk into babies.”
Winston Churchill’s words articulate the enduring view that feeding babies properly must be a good thing, not just for their own health, but also for the country as a whole. The Prime Minister was referring to the welfare food scheme established under wartime emergency legislation in 1940, but his words echo earlier public health pronouncements repeated regularly by politicians, paediatricians and the press, particularly during periods of national anxiety.
“…the unwholesome diluted milk of unhealthy badly-fed cows; such is the nourishment afforded to thousands of children on this day of an enlightened age, in this capital city of a civilised country…” (Editorial, Lancet 1858)
“Pure unadulterated breastmilk from its mother is the best food that can be supplied to the infant.” (Charles Routh, Author of Infant Feeding and its Influence on Life, 1879)
“Without clean milk there will be continued death and unfitness; the moral is that every effort should be made to get clean milk…. Then and only then will this great national problem be satisfactorily solved.” (Editorial, British Medical Journal, 1903)
Milk has always been at the heart of debates about infant welfare, whether because of its harmful or beneficial properties. Seeing milk as a panacea or a poison depends as much upon its source as social context. Biologically cows’ milk is for calves and human milk is for babies, but cows’ milk has often been used to feed babies when human milk has not been available, for biological, medical or social reasons. The ambiguous status of humanised cow’s milk, provided by successive governments as a part of infant welfare initiatives, perpetuates a tension between breast and bottle feeding that can be perceived throughout the history of infant feeding from antiquity.
This is no surprise, of course, because for the first few months of life a child’s health, growth, and indeed survival, is almost entirely dependent on the quality and quantity of the milk it receives. Breastfeeding can be a matter of life and death. Apart from supplying all the nutrition a baby needs for about six months, human milk protects against some infections, while suckling delays the return of menstruation, thereby promoting birth spacing, with health and social advantages to both infant and family. These virtues of breastfeeding may not seem that important in a country with good health services, ready access to contraception and clean artificial milk formulas. However for the vast majority of the world’s children, more than four-fifths of whom are born in the developing world, they can be critical. UNICEF has estimated that a universal practice of breastfeeding for at least six months could save some 1.5 million lives each year worldwide.
Infant feeding in the 19th century
Children born now in many countries are exposed to many of the same environmental conditions as those that characterised the towns and cities of Europe and North America a century or more ago. During their rapid urbanisation and industrial development, large families, high rates of female employment in poorly paid and casual work, poor sanitation, domestic over-crowding, adulterated and contaminated milk all posed enormous threats to the survival of the newborn in the nineteenth century. The fate of babies not nursed by their mothers was starkest for those who were abandoned or orphaned. Infant mortality was more than 90% in some foundling hospitals and “want of breastmilk” was frequently recorded as the cause. While physicians, philanthropists, politicians and public health professionals were unanimous in their support of breastfeeding, they were forced to search for substitutes for mothers’ milk, to save those infants whose mothers would not or could not nurse them.
Wet nursing was a traditional alternative and the next best thing. In Paris, a city that depended on a work force of young women as artisans in its numerous small workshops and local trades, wet nursing became part of the local economy. Newborn babies were sent to wet nurses in the countryside, under the auspices of the Bureaux des Nourrices, which facilitated and later regulated the wet nursing business. Paris was described as a “city without babies”. A welcome source of income passed with these infant wards to poor rural communities, and weaned infants returned to their working mothers a year or so later. However, many babies did not survive: despite receiving payment, some wet-nurses were unable to sustain lactation or favoured their own children above their wards. Consequently, crèches were established in the 1840s in an attempt to reverse this situation, by helping working mothers to nurse their babies during the course of their employment. But these had relatively little impact on infant mortality rates, which remained as high as 250 per thousand or more (national average infant mortality rates at this time in England were about 150 per thousand; today they are under 5 per thousand). The association between artificial feeding and infant mortality was given numeric force with the collection of vital statistics, which underlined the close association between the two.
Scientific infant care
The political satirist Honoré Daumier chose to represent the new, second French Republic (1848-70) as an androgynous mother-figure nourishing and educating her children. Milk symbolised care, growth, strength and learning.
Figure 1
This period saw the start of the incorporation of science within clinical medicine and hygiene, with the adoption of the microscope, stethoscope and weighing balance. Rousseau’s earlier call, in the eighteenth-century, for the emancipation of child rearing, with the promotion of maternal nursing and the abandonment of swaddling, was now eclipsed in the course of the early and mid nineteenth century by the rise of scientific child care. The application of chemistry and microscopy to an understanding of the composition of milk laid the foundations for the development of artificial feeds, and food technology, and nutritional science began to inform the theory and practice of infant feeding. By the end of the century simple infant milk formulas were becoming available, and wet nursing was undermined by dry nursing.
Thus, during the second half of the nineteenth century the focus on the composition and quality of milk began to shift towards an interest in the development and growth of the baby. Noting these continental advances, Charles Routh, a London obstetrician, wrote in 1860:
“The direct and baneful agency of want of good breast-milk may be inferred from the table (fig 2), from which it appears that the longer the supply of breast-milk and the more exclusively it is given the better the child is developed and vice versa.”
Figure 2
However while dividing babies into categories of ‘well-developed’, ‘medium-developed’ and ‘badly-developed’ revealed the potent influence of milk, weighing them added some objective; ‘scientific’ measurement. The weighing balance, used initially to determine the viability of the newborn, became an instrument to assess the milk intakes of babies, out of which arose the equation of growth in weight with health. Pioneered in the Pavillon des Enfants Débiles (newborn nursery of the Paris maternity hospital) for the care of small and premature babies, the balance and growth chart joined the thermometer and temperature chart as key tools in the care of the vulnerable newborn. Pierre Budin, obstetrician in charge of the Pavillon, wrote in 1907:
“When babies develop normally they put on weight regularly and of a quantity more or less according to their age – this is a general rule. When the curve of weight gain of an infant is good, one can conclude that it is in an excellent state of health, and is in no danger; if it is unwell one knows that the weight goes down.”
The achievements of ‘scientific’ child care within the hospital ward and clinic inspired the establishment of infant welfare clinics designed to safeguard the growing infant in the community. Giving impetus to the puériculture movement that had arisen following France’s disastrous defeat by the Prussians in 1870-1, they brought together politicians, obstetricians and paediatricians in a common goal of improving maternal and child health through welfare reform and new public health initiatives.
By the early twentieth century the nutritional quality and cleanliness of milk formulas were such that they were considered relatively safe alternatives to breastfeeding. They found a place in the consultations des nourrissons, pioneered by Budin in the 1890s, upon which were modelled the gouttes de lait and infant milk depots that were established in many other European countries and North America in the early 1900s. Designed to provide mothers with ‘pure clean milk’ on condition that their babies were weighed regularly, the urban milk depots were promoted as an answer to a persistently high infant mortality rate (still well over 100 per thousand live births in many countries), which was perceived as a threat to the future of the imperial powers. During the first ten years of the twentieth century (sometimes called the ‘decade of welfare’ on account of a raft of legislation in this area) infant feeding became a political question in many of these countries and drew together politicians and public health professionals, dedicated to fighting the perceived threat to the national health of ‘physical deterioration’, ‘degeneracy’ and ‘depopulation’.
Infant feeding in the 20th century
Breastfeeding rates remained relatively high in Great Britain, particularly amongst the poor. Surveys by medical officers of health in England at the start of the twentieth century reported figures of around 80% during the early months of life. Breastfeeding was free, and although cheap infant milk formulas were coming onto the market, access to them was often through a physician (and therefore expensive when every consultation had to be paid for before the NHS). After the First World War the availability of dried milk and relaxation of medical control of infant feeding made safer artificial feeds more widely used and hygienic bottle feeding more popular.
Infant mortality rates started to decline rapidly around the turn of the century (there remains much debate among historians over the precise causes of this – possible factors include falling fertility, improving care of mothers and babies before and after birth, better housing and domiciliary water supplies, more hygienic domestic practices, and cleaner streets reducing exposure to flies – (thought then to be a source of infantile summer diarrhoea). Consequently by the 1920s infant feeding had ceased to be a pressing political issue. Paediatrics had come of age, in part through the apparent success and effectiveness of the application of nutritional science to infant welfare. Scientific child care came to embrace artificial feeding, and by the 1950s, in North America particularly, some paediatricians took the view that bottle-feeding was as good as breastfeeding. Infant feeding became a matter of maternal choice.
Surveys of well babies demonstrated that bottle-fed infants could thrive as well as breastfed, reinforcing the credibility of infant milk formulas and the value of growth charts. Sequential weighing with the use of charts to monitor growth became the justification for infant welfare clinics. Compiled largely from data collected in these clinics, such growth charts were based on small numbers of children. As infant welfare and health surveillance grew there arose a demand for ‘growth standards’ based on large populations.
The developing world
In the developing world the story was different. The mass production of artificial infant milks and their promotion outside Europe and North America from the 1930s, with the creation of international markets, had disastrous effects. In the societies of sub-Saharan Africa and the Far East, where clean water was not always available, artificial milks proved fatal. Where breastfeeding had never previously been questioned in these cultures, where it was a critical factor in child health and survival, bottle-feeding killed babies. It took an international movement, initiated as early as the 1930s by a few alert and determined health workers and activists in Africa and Asia to publicise this scandal, which eventually grew into worldwide condemnation of some infant milk companies that continues to this day. The essential role of breastfeeding in these societies, and its crucial relationship with infant growth, health and development was made starkly obvious, and has been a major motivator of concerted research into lactation, infant nutrition, reproduction and child care.
The infant growth chart became an essential tool in such research programmes and in the battle to draw attention to the fatal effects of formula-feeding. It was increasingly adopted in international child health initiatives in the developing world, to chart not just body weight but also the ‘road to health’. Infant growth rate became as powerful an index of success or failure as infant mortality rates. By the 1970s it was becoming apparent to public health professionals that formula-fed babies in the developing world grew ‘faster’ than breastfed, while babies in the developed world, weaned early onto inadequate alternatives to mother’s milk, failed to thrive. But ‘faster’ was not necessarily better, and by the 1980s the search started for universal growth standards, applicable to all babies everywhere.
Policy and practice then and now
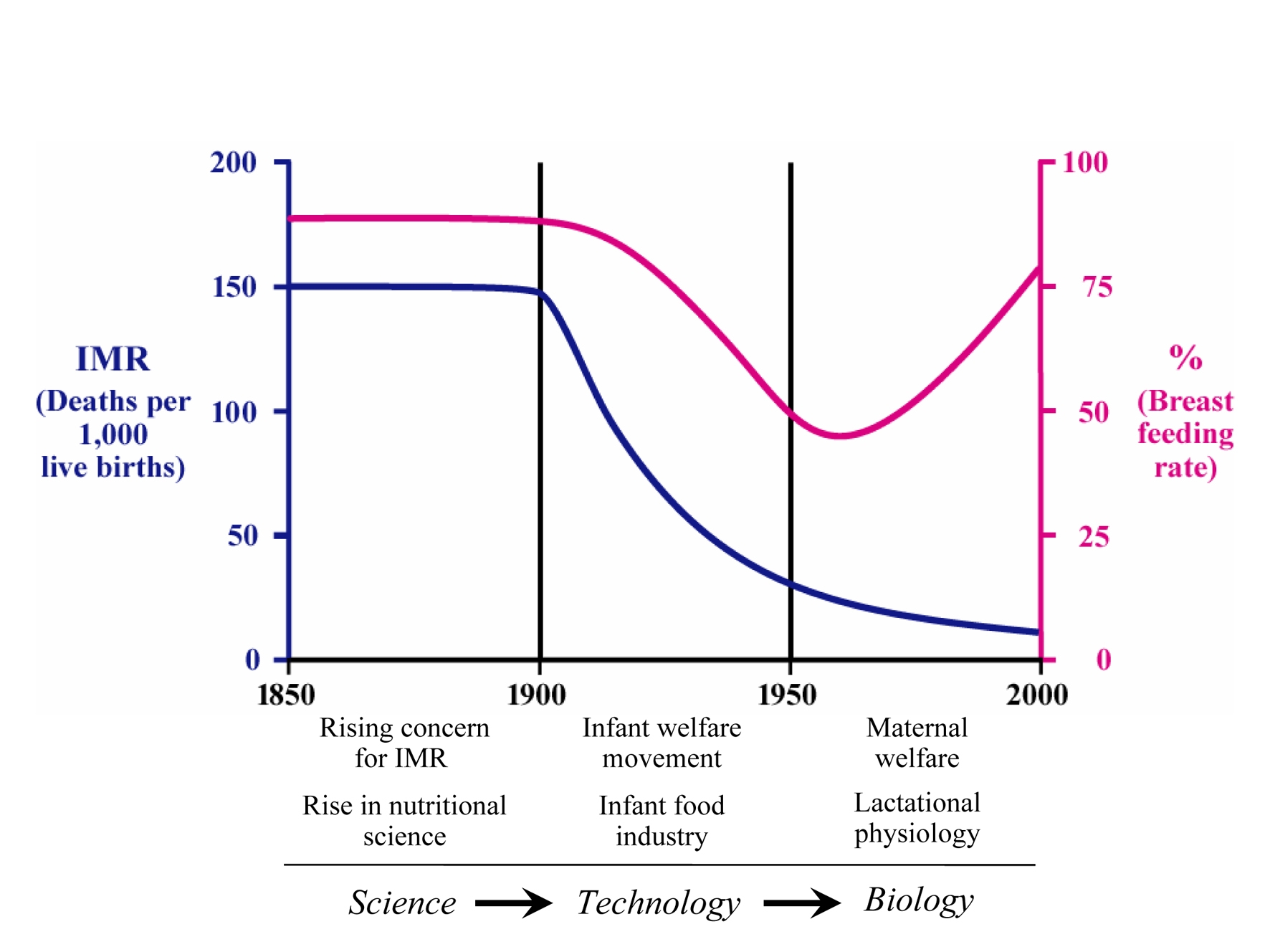
These initiatives for evaluating the health, growth and development of infants in the developing world, while informing and empowering international agencies, coincided with a waning of mechanistic physico-chemical approaches to infant nutrition and a rise in the application of the insights of physiology and biochemistry to medicine. Biology has replaced food technology as the dominant framework for thinking about infant nutrition and its practice (fig 3). The ‘disadvantages’ of bottle feeding have been redefined, with an emphasis on the protective effects of breastfeeding, and the infant milk formula industry has begun to retreat under attack from public health activists. Global health programmes, such as the UNICEF Baby Friendly Initiative and WHO Innocenti Declaration, assert the fundamental importance of breastfeeding for child health. Nevertheless the habit of breastfeeding is not quickly replacing the habit of bottle-feeding, at least not amongst the mothers whose babies are likely to benefit most.
Figure 3
In this country breastfeeding may no longer be a matter of life and death. With an infant mortality rate now of around 5 per 1000, this small number of deaths is mainly due to extreme prematurity and congenital abnormalities, conditions that have little to do with feeding. Nevertheless breastfeeding has assumed a new public health importance, one that echoes the concerns of policymakers of the past, but with a new emphasis (in some of the most developed countries) not so much on survival, but on lifelong health. Human milk contains unique substances (such as specific long chain fatty acids and oligosaccharides – complex sugar compounds) that it is claimed are associated with superior IQ, neurodevelopment and protection against infection. The adage that child health is the foundation of adult health is now articulated in the ‘early origins of adult disease’ hypothesis and so, conversely, that a healthy start sets the child on the optimum trajectory for a life free of chronic disease. Infant mortality rate is no longer a useful or relevant index of child health in the developed world (though it remains one of the best overall public health indices of a nation’s health globally), and has been replaced by infant growth: deaths per thousand live births have been superseded by grams of weight gained per month.
The new WHO growth charts were introduced in the UK during National Breastfeeding Awareness Week (10-16 May) 2009. These ‘growth standards’ are based on measurements of more than 6,000 healthy breastfed children worldwide. Their adoption and promotion is predicated on the principle that growth, indeed health, in infancy is largely determined by how babies are fed and that the growth trajectory of the healthy breastfed infant is a gold standard to which all the world should aspire for its infants. The ‘rapid’ early growth often experienced by formula-fed babies, and on which previous growth charts had been based, is not necessarily optimal. The shape and pattern of the growth curve of the breastfed baby differs from that of the bottle-fed in being less steep, a characteristic which may well have implications for the burgeoning number of children that are destined to be overweight and obese (whose ‘rapid’ growth as babies was previously regarded as ‘healthy’ on the older growth charts). The ‘slower’ growth of the breastfed baby, compared to that of the bottle-fed baby, seems to be a good thing and a defence against obesity, diabetes, hypertension and chronic heart disease in later life.
A resurgence of breastfeeding?
Breastfeeding rates in the UK have risen from a nadir in the 1960s and 70s, but remain among the lowest in Europe. While 70% of mothers feed their babies themselves at birth, less than half of that figure still does so at three months. A Witness Seminar convened by the Wellcome Trust in 2007 brought together a group of professionals and lay people who had been involved with the science, practice and promotion of breastfeeding during the last thirty years or so, to discuss whether or not there has been a resurgence of breastfeeding as a result of the growing recognition of its benefits to mother and baby. The meeting was both a metaphor and microcosm of how breastfeeding is seen by different people, and made clear that it is still a very live and contentious issue. Breastfeeding rates have been creeping up, but few felt that this could be called a resurgence.
At this Witness Seminar, the disjunction between the work of reproductive and lactational physiologists mirrored that between obstetricians and neonatologists, and between paediatricians and midwives, revealing a gender divide that might be said to begin and belong to the moment of birth. Those most intimately involved with the act of birth – mother and baby – are cared for by midwives and doctors who, if not both in attendance, still exercise influence on mothers’ decisions to breastfeed. ‘Naturalisation’ of child birth, returning it from obstetricians to women, and the activities of many breastfeeding support groups, have helped to de-medicalise professional thinking about infant feeding and to educate the public. But there is a long way to go before breastfeeding rates reach levels comparable to those a hundred years ago.
Breastfeeding, so vital and fundamental a part of the biology of early life, has potent social and political meaning because of its power to influence the life course of children and the risk of diseases that will add an increasing burden to our health services. The nature of milk may be ambiguous, and the history of infant feeding seen as a battle between the promises of technology, the pressures of commerce, and the promotion of biology. Health messages about the positive advantages of breastfeeding require constant re-articulation, and while its prime justification may no longer be infant survival but lifelong health, its positive value for mother, child and society as a whole, remains as strong and true as ever.