With January 2011's Health and Social Care Bill, following the financial settlement in October's Comprehensive Spending Review (CSR), the major elements of Coalition policy towards the National Health Service (NHS) are clear. The Tory election pledge of maintaining a real term increase in expenditure has apparently been fulfilled, thus underscoring the commitment which is a keystone of the Cameron/Osborne project. Meanwhile Health Secretary Andrew Lansley has developed a reform package he characterises as 'liberation' from central targets and excessive bureaucracy which will achieve 'equity and excellence'. Does the Lansley programme represent 'revolution' or rather a continuation of the New Labour trajectory? And what might consideration of the NHS's past experience suggest about likely points of pressure and tension?
The purpose of this paper is to consider where these current proposals stand in the longer history of the NHS. The discussion begins by identifying forces of continuity and change which shape the present policy agenda, then assesses the funding package in the light of past trends. Historical contextualisation of the reform proposals divides into two sections: firstly, the 'equity and excellence' elements - the organisational changes to commissioning arrangements and related plans to find efficiency savings; secondly, the 'liberation' menu, including the relinquishing of central controls over target setting and commissioning, and reforms to the National Institute for Clinical Excellence (NICE).
Recent Conservative policy towards the NHS was coloured by the aim of 'detoxifying' their brand. Electoral defeats in 2001 and 2005 were accompanied by unpopular market-oriented proposals, such as tax breaks for private medical insurance and subsidies for paying patients. Thus one of Cameron's first actions as leader in 2006 was to commit the Tories to the 'noble vision' of traditional NHS principles. This was a return to the pragmatism of the early Thatcher period when electoral caution tempered reform zeal: in then Chancellor Nigel Lawson's oft-quoted phrase, the NHS 'is the closest thing the English have to a religion', and highly politically sensitive. It was perhaps also strategic, for the constituency which makes the greatest use of the NHS, older people, tends disproportionately to vote Conservative and has enjoyed other protections in the austerity package. Then Prime Minister Tony Blair and Chancellor Gordon Brown had broadly followed the Thatcher/Major programme, maintaining the internal market, pursuing private finance in capital projects, and encouraging more pluralist provision. The associated political rhetoric of localism, choice and patient empowerment was therefore compatible with Conservative discourse. Finally, continuity was justified as a respite for health professionals from 'pointless and disruptive reorganisations' and sealed with a promise not to 'allow any meddling with existing local or regional structures', according to a 2008 Conservative Party document.
At the same time several drivers of change emerged. First, a platform of holding steady offered little scope for an incoming minister with extensive experience of the health brief, who now wanted to make his mark. Indeed, only electoral caution may explain the absence from the April 2010 Conservative manifesto of Lansley's planned abolition of Primary Care Trusts (PCTs), unveiled in July's White Paper. Second, populist electoral considerations seem likely to have lain behind some policies, such as the departure from existing rationing strategies through a new cancer drug fund, and opposition to planned hospital closures disliked by local pressure groups. Third, and crucially, the government's decision to pursue early fiscal tightening in response to the financial crisis elevated the urgency of achieving payroll savings by reducing administrative staff.
In the CSR the Coalition committed the bare minimum necessary to honour its undertaking of a real increase, with the NHS budget for England increasing by 0.3% between 2011/12 and 2014/15. However, 'real' growth is dependent upon the course of inflation, and recently revised assumptions by the Office of Budget Responsibility instead imply a small decrease. The NHS will also be required to allot a small proportion of its budget to support local authority social care expenditure (the background to which is approximately a 26% decrease in government funding to councils).
This settlement contrasts markedly with the general pattern of post-war funding under various governments (Figure 1). Over the NHS's first sixty years the mean real term annual increase was just under 4%. It was accepted within the Department of Health, even during the parsimonious early 1980s, that real increases ought to be at least around 1%, given the rising morbidity burden of an ageing population. Other cost-drivers included the need to meet mounting public expectations and demands of new technologies and drugs. Recent years saw a steeper upward trend, following Blair's promise to raise British expenditure to the European average. Recognition of the gap between the UK and other advanced industrial nations in health expenditure dates back at least to the 1970s, but became politically contentious under New Labour. Complacent assumptions that this gap simply represented the NHS's greater cost effectiveness were shaken by novel measures of health outcome, such as cancer survival rates and mortality amenable to health care, in which Britain lagged behind its peers. Thus policy shifted to favour significantly enhanced inputs, and between 1999/2000 and 2004/5 the five-year moving average of real spending increase climbed from about 2% to 8%.
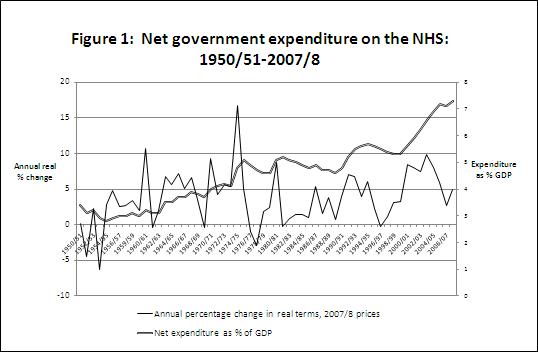 |
| Source: Underlying data from Gavin Thompson, NHS expenditure in England, House of Commons Library, Standard Note SN/SG/724, 16; note that NHS-specific weighted adjustments to the GDP deflator will produce different annual real percentage changes, see Appleby, further reading. |
On these counts the CSR settlement augurs a phase of stringency with only few parallels in NHS history. One such period was the Churchill/Eden governments of the early 1950s, which saw its largest real decreases. Behind these lay the anxieties of the Treasury, which mistakenly assumed that the newly created service would prove an intolerable strain on national finances. The other notably low-spending period followed the mid-seventies oil shock and fears of a fiscal crisis of the welfare state. The early 1970s had seen high expenditure in response to wage claims from the NHS workforce, while the 1974/5 peak represented the transfer to the NHS of local government health responsibilities following Secretary of State for Social Services Keith Joseph's 1974 reorganisation. From 1976/7 the Callaghan government registered two years of real decrease as it grappled with the sterling crisis and the IMF loan. Thatcher initially boosted spending, in response to poor labour relations and social tensions in the early 1980s, but then embarked on a sustained policy of tight settlements coupled with management reform.
The major difference between the current phase and earlier episodes is that the NHS now starts from a higher base. In the early 1950s it consumed around 3% of GDP, in the 1980s around 5% but by the time of Blair's departure, about 7% (Figure 1). Moreover four years of standstill is hardly the 'arctic' scenario of real reductions which some commentators modelled when the scale of the UK budget deficit became clear. However, those who argue that overall funding levels do matter will worry on two counts. First, past experience of periods of higher unemployment in the 1930s and 1980s has demonstrated that joblessness is associated with rising morbidity and thus increased demand. Strain is particularly likely to fall on mental health services, which in some areas have been under pressure: in London for example this was a theme of King's Fund reports through the 1990s and 2000s.
Second, it potentially undermines the UK's capacity to improve its health outcomes relative to other countries. In respect of health expenditure as % of GDP, by 2008 the UK (8.7) still lagged behind the OECD mean (9.0), and despite the years of plenty remained below France (11.2), Switzerland (10.7), Germany (10.5), Canada (10.4), the Netherlands (9.9), Sweden (9.4), Italy (9.1) and Spain (9.0). The lowering of the overall settlement with these differentials still in place will provide a high stakes testbed for assessing the importance of total spend to comparative health measures. However, future outcomes will depend not simply on the Treasury's financial plans but on the structural reform which will accompany them. Indeed the success of the latter may be compromised by the former: Secretary of State for Health Kenneth Clarke's introduction of the internal market was eased by more buoyant funding following the restraint of the Thatcher years, with an average real increase 1990/1-1994/5 of 5.5%. What else can historical contextualisation suggest?
3.1 Commissioning structures The most fundamental reform will be the abolition of the PCTs, the 'purchaser' bodies responsible for commissioning of services from 'providers' (predominantly hospital trusts). Where the Tory manifesto spoke generally about transferring budget-holding and commissioning responsibilities to GPs, the Bill provides for practices to combine into consortia for this purpose. Also to disappear are Strategic Health Authorities (SHAs), the distant heirs to the regional governance structures which once dominated the NHS. Today their responsibilities include distributing finance, commissioning specialist services and supervising public health. In their place will come an independent NHS Commissioning Board to oversee the behaviour of consortia, while public health will move back to local government, where it sat before 1974. In abolishing the PCTs the Conservatives are returning to the thrust of policy developed in the mid-1990s during the early phase of the internal market. When they left office they had been presiding over a gradual increase in GP fund-holding, where practices became independent of the District Health Authorities (DHAs) which had initially held responsibility for purchasing. The policy had been controversial and only about half of GP practices had opted out by 1997: there had been much vaunted fears that a two-tier system would result, favouring the fund-holders.
Labour initially halted the policy, replacing purchasing with more consensual service agreements. But under Secretary of State for Health Alan Milburn the NHS moved back to market. PCTs were created as a new tier of independent trusts in place of the DHAs and commissioning processes were strengthened, now with a tariff system based on 'payment by results'. Practice-based commissioning was fostered within the PCTs, specifically to bring the judgements of 'frontline' doctors to the fore. Thus while the Tories are picking up where they left off in 1997, they are also taking forward New Labour's approach. History appears to augur caution here, for if the permissive and gradualist steps of the last twenty years have led only haltingly to GP commissioning, then it may be that many doctors have little appetite for these new duties. A King's Fund survey has underscored this, with about 40% of doctors disagreeing with the proposition that the reforms will improve the quality of care, and only 46% confident that GPs have the local capacity to lead consortia. GPs may also resent blame falling on their shoulders if failures arise as a result of austerity measures.
That said, if managed carefully the outcome may be evolution not revolution. This would not be the first time the profession has objected to change, only to accede when it was imposed on them: there were similar dire warnings at the inception of both the NHS and the internal market. And GPs have gained personally from the Blair funding injection, with salaries outpacing their European peers, so militancy may be muted. Finally, GPs will be at liberty to employ outside bodies to conduct their commissioning. The result though, may simply be musical chairs as the remnants of PCTs restructure, particularly if projections of slender profit margins deter private sector actors.
3.2 Reducing the managers GP compliance is not the only crucial variable. The other is the planned cull of NHS administrative staff due to the financial crisis. The CSR assumes a £20 billion annual efficiency saving, and the abolition of the PCTs and SHAs is presumably seen as a shock therapy which will achieve this.
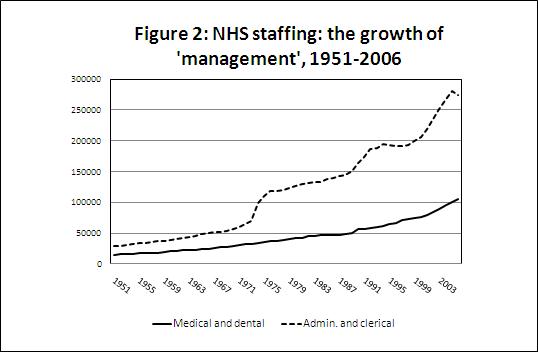 |
| Source: Underlying data from Office of Health Economics, Compendium of Health Statistics, 2009 Table 3.3 'Number of staff employed in NHS hospitals and community services by category, UK, 1951-2006' |
The rise in managerial numbers (broadly defined as administrative and clerical staff) has been a long process (Figure 2) arising largely from earlier Tory policies: the 1974 reorganisation, when administrators entered the newly created health authorities; the introduction of general management following the 1983 Griffiths Report; and the increase accompanying the internal market with its associated bureaucracy. The upward spike under Labour therefore continues a long-run trend, now fuelled by spending increases. Is this fat which can be safely trimmed without damaging performance? History suggests caution about this assumption, because past experience has seen structural change depriving the service of experienced managers. In 1974 for example, the reorganisation prompted an exodus of the senior cadre of Medical Officers of Health, and of top-level hospital administrators; this meant that although there were more hospital managers the new blood worked less effectively with clinicians. By December 2010 there was evidence that this was happening again, now at the level of PCTs. Already these are threatened with 'meltdown' as staff opt for retirement or resignation before abolition.
While there may be hyperbole in forecasts of organisational chaos, there is surely a danger that rapid structural change will weaken commissioning capabilities. To establish whether this is a serious risk, we need to consider the record of the different 'purchasing'/'commissioning' bodies over the last twenty years.
3.3 Commissioning's historical record Reflecting in 2008 on the NHS's 60th anniversary, Kenneth Clarke observed that: '20 years on we are still in the position where commissioning is the weak point in the whole thing ... if one day, subsequent generations find you cannot make commissioning work - then we have been barking up the wrong tree for the last 20 years.' Clarke had boldly launched the internal market in 1990 without detailed piloting, on the assumption that purchasers would learn by doing; now he was candidly acknowledging the mixed record of this experiment.
Evaluations conducted from the mid-1990s adjudged the first phase of the internal market to have been neither as bad as doom-mongers predicted, nor as positive as its champions forecast. Verdicts on Labour's quasi-market were better, at least for acute care. For example, areas with greater competition between providers saw steeper falls in mortality from heart attacks, and while equity of access remained broadly unchanged, inequalities were reducing for some elective procedures. Patients also valued choice, though few drew on the new NHS information systems. However, recent assessments of commissioning's record highlighted key weaknesses. It is the providers, the hospitals, which have attracted better calibre managers, while the PCTs have been too passive towards them, failing to use their leverage to raise quality or to pioneer new service patterns. There also remain considerable geographical variations in both health outcomes and in costs of contracts, which indicate persistent inequity and inefficiency. For example, after weighting for population there is a two-fold difference in PCT spending on cancer in-patients in England, and a 2.5-fold range in mental health expenditure. Finally, departmental information on the transaction costs of commissioning is lacking, which prevents meaningful comparison of its cost effectiveness against that of planned resource allocation. External analysts suggest that around 13.5% of the NHS budget and about a quarter of its staffing was devoted to such costs since 1997.
Reviewing these issues in 2010 the Commons Health Select Committee voiced the policy option of abandoning the purchaser/provider split. The Brown government rejected this, and clearly the Coalition thinks the same. Yet past performance provides no firm assurance that handing the reins to GPs will deliver the desired improvement. Moreover, proposals to reintroduce price competition between providers alongside the tariff system will place even greater onus on commissioners, if quality is not to suffer.
4.1 Independent management The Bill proposes two bodies which will limit 'the powers of Ministers over day-to-day NHS decisions'. The existing regulator, 'Monitor', will have powers of licensing, financial oversight and enforcement when NHS bodies fail, while a new NHS Commissioning Board will allocate resources, manage commissioning, promote patient involvement and reduce inequalities. Relinquishing Whitehall 'command and control' has long figured in political rhetoric, but this represents a radical handover. Policy debate about an independent board for the NHS extends through its history, with solutions such as a BBC-style Board of Governors touted. Earlier proposals always foundered on the problem pithily articulated in 1966 by Enoch Powell, Minister for Health 1960-63, as: 'the constitutional principle that the proceeds of taxation must be expended by those who are representatives of the taxpayers. ... the whole idea of non-ministerial management ... is a chimera.'
The closest the NHS came before was in the mid-1980s, when Secretary of State for Social Services Norman Fowler sought to separate managerial from strategic decision-making, the former deemed essentially practical and the latter inherently political. A NHS Management Board was established, though lacking statutory independence, with an industrialist, Victor Paige, as Chief Executive. The experiment was rethought when Paige resigned, frustrated that political concerns could not be disentangled from managerial imperatives. The companion Strategic Board quickly withered, and the Minister of State was brought in to chair the Management Board, in acknowledgement that de-politicisation hadn't succeeded. Nonetheless, it has remained an enticing policy goal. Depoliticising the running of the NHS could genuinely free executives to manage, and substantially absolve ministers from responsibility for stewardship of the service. However, the 'Enoch Powell problem' is hardly likely to disappear, and Fowler's experiment also occurred in a period of tight financial settlements and turbulent health politics. A return of accountability to Parliament may quickly turn into a priority if unfavourable headlines appear and are exploited by the opposition. Moreover, as Powell also warned, an independent body seen to be failing would become a source of opposition, castigating the government for under-resourcing.
4.2 Have targets worked? The Conservative plans include 'discarding ... certain top-down targets' in favour of 'clinically credible' measures approved by professionals. This departs from New Labour's use of target setting to ensure spending departments delivered value in return for increased inputs. The approach built upon the audit culture fostered by new public management reforms in the 1980s, which demanded that meaningful performance indicators should be developed and monitored. Making these transparent, typically in league tables, would, in theory, incentivise the 'producers' (teachers, doctors) and empower the 'consumers' (parents, patients). Targets were disliked by public sector employees who felt their integrity was impugned and resented the accompanying bureaucracy. Effectiveness was also questioned, with concerns that providers were gaming the system, or that over-attention to targeted areas weakened performance in others. Intriguingly though, research on recent historical trends in that most sensitive area - hospital waiting lists - cautions against abandonment of the 'targets and terror' strategy. Political devolution since 1999 created a natural laboratory in which the outcomes of different policies adopted in the UK's constituent nations could be assessed. Comparison of the pace of decline of waiting lists in England, Scotland and Wales is instructive, for only England required that funding be attached to the meeting of publicly reported targets. Yet despite having the lowest rates of per capita expenditure, nursing and medical staff, England has outperformed the other nations in driving down waiting times. Clearly these gains cannot be detached from the funding boost or longer term efforts to improve managerial quality, yet there is a strong case that England's superior performance in this electorally highlysensitive respect is attributable to central target setting and public exposure of outcomes.
4.3 Disempowering NICE? The Bill also puts NICE, the body responsible for guiding the NHS on new technologies, on a statutory footing under the regulation of the Secretary of State. However, Conservative policy documents have hinted at dilution of its powers, with two key justifications. First, there are concerns about NICE's method of assessing cost effectiveness, the Quality Adjusted Life Year (QALY) score. This is a measure of therapeutic value which permits dispassionate comparison of different treatments, and subsequent NICE guidance is intended to aid commissioning decisions. The new proposal is to incorporate additional assessment of social value and benefit, partly by moving decision-making power on purchasing away from NICE and to the 'front line'. The public interest objective is to avert controversy (often media fuelled) over expensive drugs for which NICE decisions have appeared too brutal. Second, Conservatives worry that NICE rulings can disadvantage the UK's pharmaceutical industry, with the risk that research and development is undermined and business dynamism inhibited. The mooted solution is a joint pharmaceutical industry, NICE and Department of Health steering group. Accordingly NICE's duties are now to assess the 'broad balance' of 'benefits and costs', mindful of the 'desirability of promoting innovation'. While the problem of balancing public and industry interests in NHS pharmaceutical purchases is almost as old as the service, this may signal some diversion in the policy trajectory. Formal mechanisms go back to the Voluntary Price Regulation Scheme (VPRS), begun in 1957, under which ministers sought to control burgeoning drugs expenditure through a consultative process with the industry on fair levels of profit. Renewal of the Scheme in the 1960s strengthened the NHS's hand, for example by forcing restraint on promotional spending on branded drugs. A tougher line emerged in the mid-1980s when Fowler imposed a list of costly branded drugs which could be safely substituted by cheaper generic products. And eventually the search for a scientific method of assessing cost effectiveness led to the creation of NICE under Secretary of State for Health Frank Dobson, with the introduction of QALY as a rationing instrument.
History suggests that efforts to respond to public, media and industry concerns by weakening NICE's hand may come under pressure. In the NHS's early years it was the Treasury and the Public Accounts Committee which were most eager to rein back drugs cost and made the running in policy debates which led to the VPRS. Similarly, the selected list of the 1980s was brought in at the height of Thatcherite spending restraint. Thus it is possible that in the current climate the policy goal of making rationing more socially and industrially responsive may fall prey to similar forces.
In the medium and longer terms, historical context points to a combination of pressures which might challenge the Coalition programme.
J. Appleby, 'Government funding of the UK National Health Service: what does the historical record reveal?' Journal of Health Services Research and Policy, 4, 2, 1999, 79-89.
S. Connolly, G.Bevan, N.Mays, Funding and performance of healthcare systems in the four countries of the UK before and after devolution.London, Nuffield Trust, 2010. House of Commons Health Committee, Commissioning: Fourth Report of Session 2009-10, Volume I.
M. Gorsky, 'The National Health Service at 60: a review of the historiography', Social History of Medicine, 21, 3, 2008, 437-60. R. Klein, The New Politics of the NHS: from Creation to Reinvention, Oxford: Radcliffe Publishing, 2006.
E. Powell, A new look at medicine and politics., London, Pitman Medical Publishing, 1966. C. Smee, Speaking truth to power, two decades of analysis in the Department of Health. Oxford, Radcliffe Publishing, 2005.
N. Timmins ed., Rejuvenate or retire? Views of the NHS at 60. London, Nuffield Trust, 2008. C. Webster, The National Health Service: a Political History. Oxford: Oxford University Press, 2002.
Sign up to receive announcements on events, the latest research and more!
We will never send spam and you can unsubscribe any time.
H&P is based at the Institute of Historical Research, Senate House, University of London.
We are the only project in the UK providing access to an international network of more than 500 historians with a broad range of expertise. H&P offers a range of resources for historians, policy makers and journalists.